


 Porcelain Veneers
Porcelain Veneers Teeth Whitening
Teeth Whitening Bonding
Bonding Tooth Colored Fillings
Tooth Colored Fillings Orthodontics
Orthodontics Gum Contouring
Gum Contouring Fillings
Fillings  On lays and Inlays
On lays and Inlays Crowns and Bridges
Crowns and Bridges Denture
Denture Extractions and Bone Grafts
Extractions and Bone Grafts Dental Implants
Dental Implants Periodic Checkups
Periodic Checkups Scaling and Root Planing
Scaling and Root Planing  Custom Night and Sports Guards
Custom Night and Sports Guards Snoring and Sleep Apnea
Snoring and Sleep Apnea Root Canal Treatment
Root Canal Treatment  Sealants
Sealants  Routine Checkup
Routine Checkup Fluoride Application
Fluoride Application Extractions
Extractions Space Maintainers
Space Maintainers Porcelain Fused Metallic Crown
Porcelain Fused Metallic Crown Dental Counseling
Dental Counseling Smile Makeover
Smile Makeover Neuromuscular Dentistry
Neuromuscular Dentistry Sedation Dentistry
Sedation Dentistry Laser Dentistry
Laser Dentistry Digital Dentistry
Digital Dentistry Relaxation Dentistry
Relaxation Dentistry
The Cutting Ege @ Aesthetic Edge®
Neuromuscular dentistry is a dental treatment philosophy intended to correct a “malalignment”of the jaw at the temporomandibular joint and produce a balanced bite. The neuromuscular dentist uses several computerized instruments to measure your jaw movements and jaw muscle activity to determine the extent of your problem and to establish a “physiologic rest position” for the jaw. Here are some of the measurement techniques and procedures used:
Once the rest position of the jaw is determined, the patient undergoes extensive restorative dental procedures or orthodontics to maintain this new position.
Neuromuscular dentistry can cost from $3,500 to $25,000+ for 4-6 months to one year or more of treatment. Insurance companies typically do not cover the TMJ- related costs due to the lack of a scientific evidence base for such treatment.
According to the American Association For Dental Research’s March 3, 2010 Policy Statement on Temporomandibular Disorders (TMD) “…the consensus of recent scientific literature about currently available technological diagnostic devices for TMDs is that except for various imaging modalities, none of them shows the sensitivity and specificity required to separate normal subjects from TMD patients or to distinguish among TMD subgroups.” In other words, those who practice neuromuscular dentistry have their own standards for what are normal and abnormal readings which may lead to a “false positive” - meaning people may be told they have a TMJ problem when they really don’t, leading to unnecessary treatments.
Neuromuscular dentistry is NOT a specialty recognized by the American Dental Association. Although a variety of healthcare providers advertise themselves as TMJ specialists, treatments available today are based largely on beliefs, not on scientific evidence.
what is a neuromuscular dentist?
As the name implies, a neuromuscular dentist is concerned not only with the health of the teeth and gums, but also with the entire functional system that allows you to chew, swallow, speak, sing, kiss, or yawn – anything you do with your mouth. Specifically, that system includes the jaw joints and facial muscles used to open and close your mouth. By considering the position of the teeth in relation to the optimal function of the joints and muscles, the neuromuscular dentist seeks to restore a balanced relationship within that system for patients who are experiencing pain or reduced function.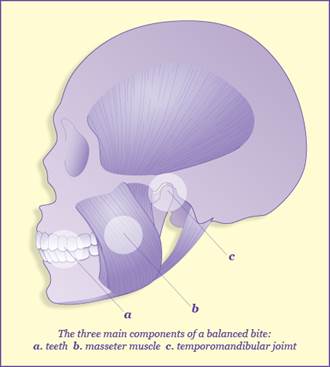
But neuromuscular dentistry is not just for people who have TMJ problems, bite misalignments, or facial pain. A patient with a well-balanced bite may still have teeth that need restoration, or desire cosmetic improvements to their smile either through orthodontics or the placement of veneers. In making any changes to the teeth, no matter how small, the neuromuscular dentist will always consider the impact on overall function and plan the proposed treatment in a way that preserves or improves the harmony of the system.
But what kind of difference can the position of the teeth really make? And perhaps more importantly, why would the bite be out of alignment in the first place?
common causes of bite misalignment
Most cases of bite misalignment are the result of an overall tooth position that requires the lower jaw to retract backwards into the face in order to make the molars fit together for chewing. Genetics can sometimes play a role in overall tooth position, but often a bite misalignment will begin with childhood allergies that initiate a habit of mouth-breathing, or orthodontics and dental restorations that don’t take the muscles and joint position into account. Tooth extraction can also cause the teeth and jaw to shift, particularly if the missing teeth are not replaced promptly.
the body’s priorities
Chewing is the most important function of our teeth, and our bodies know it. Nutrition is essential to our survival, and the ability to chew is paramount to that goal.
The nerves to the teeth are so sensitive that no matter how our teeth are positioned, the body will anticipate the best fit for chewing and adjust the position of the lower jaw accordingly – even if that means compromising the comfort and function of the joints and muscles.
In an ideal system, the teeth should hit solidly and evenly in the back but not touch in the front unless you are trying to bite into something like an apple or sandwich. The large cheek muscles, or masseters, will drive the chewing action and the TMJ or jaw joint will swing freely through the process. But when the teeth are aligned in a way that forces the lower jaw backwards, the masseter muscles are foreshortened and unable to fire correctly, causing other muscles to take over. As the lower jaw moves further back into the face, the TMJ becomes compressed. The cartilage disc that should move freely with the lower jaw as it opens and closes may become displaced and can slowly begin to change shape over time. Clicking, popping, locking, joint pain, headaches, and even ear or eye pain can often be the result of a compressed joint and compromised masseter muscles.
how does a neuromuscular dentist measure bite misalignment?
One of the first diagnostic tools a neuromuscular dentist will use to determine if your muscles and joints are functioning with your bite correctly is a muscle and joint palpation. The dentist will ask you to open, close, and clench your teeth as he or she physically feels for function in the different facial muscles and the TMJ. If it is clear that the main chewing muscles are not able to fire with clenching, then there is an imbalance in the bite. Pain in any of the palpated areas may also be an indication that something is not balanced correctly or that the muscles are being asked to function too much. Catches, locks, clicks and pops in the joints are also indications of a bite imbalance, as well as the breakdown and remodeling of the jaw joints. All these symptoms will be carefully noted during the physical exam.
Depending on the results of the exam and the reported history of pain or lack of function, a neuromuscular dentist may recommend additional computerized diagnostic testing to determine the exact amount of imbalance in the bite and what type of treatment might help alleviate pain and restore normal function. For some, a short time in a simple orthotic device combined with a regimen of self-care may be all that is needed. For others, more permanent changes to the bite, including neuromuscular functional orthodontics or full-mouth reconstruction, may be required to fully restore function and address pain.
For all dental patients, neuromuscular dentistry offers an integrated approach to health and dental treatment. Everything in the body is connected. By considering the teeth in relation to the other systems necessary to support proper function, the neuromuscular dentist focuses on building and protecting the balanced foundation necessary to create a solid bite and pain-free function for a lifetime.

